Automated outbound healthcare phone calls
SuperDial automates healthcare revenue cycle tasks like eligibility checks, prior authorizations, claim status, credentialing, and enrollment.
Book a demoSuperDial automates healthcare revenue cycle tasks like eligibility checks, prior authorizations, claim status, credentialing, and enrollment.
Book a demoBacked by leading technology investors




Built for revenue cycle teams, SuperDial's AI voice agents automate payor calls end-to-end — with results logged in your existing systems.
Book a demo
Confirm patient deductible, co-pay, and coverage details, without picking up the phone.

Confirm clinician status, credentials, and new patient acceptance directly from provider offices.

Retrieve prior auth requirements and real-time status updates from any payor.
Follow up on denied, delayed, or unpaid claims — and resolve them automatically.
Inquire about enrollment or credentialing status for new practices.
Use customizable scripting to automate any outbound payor or provider call.
See how SuperDial transformed West Coast Dental's claims process and reduced AR days by handling over 10,000 calls per month
Book a demo
SuperDial frees up revenue cycle personnel to focus on the highest possible problem-solving needs while AI handles critical but highly reptitive work like data gathering

Paul Bernard
Former CEO, Inside Desk; Current Chief Product Officer, Vyne Dental

Share the call script your team currently uses, or customize one from the templates in our portal.
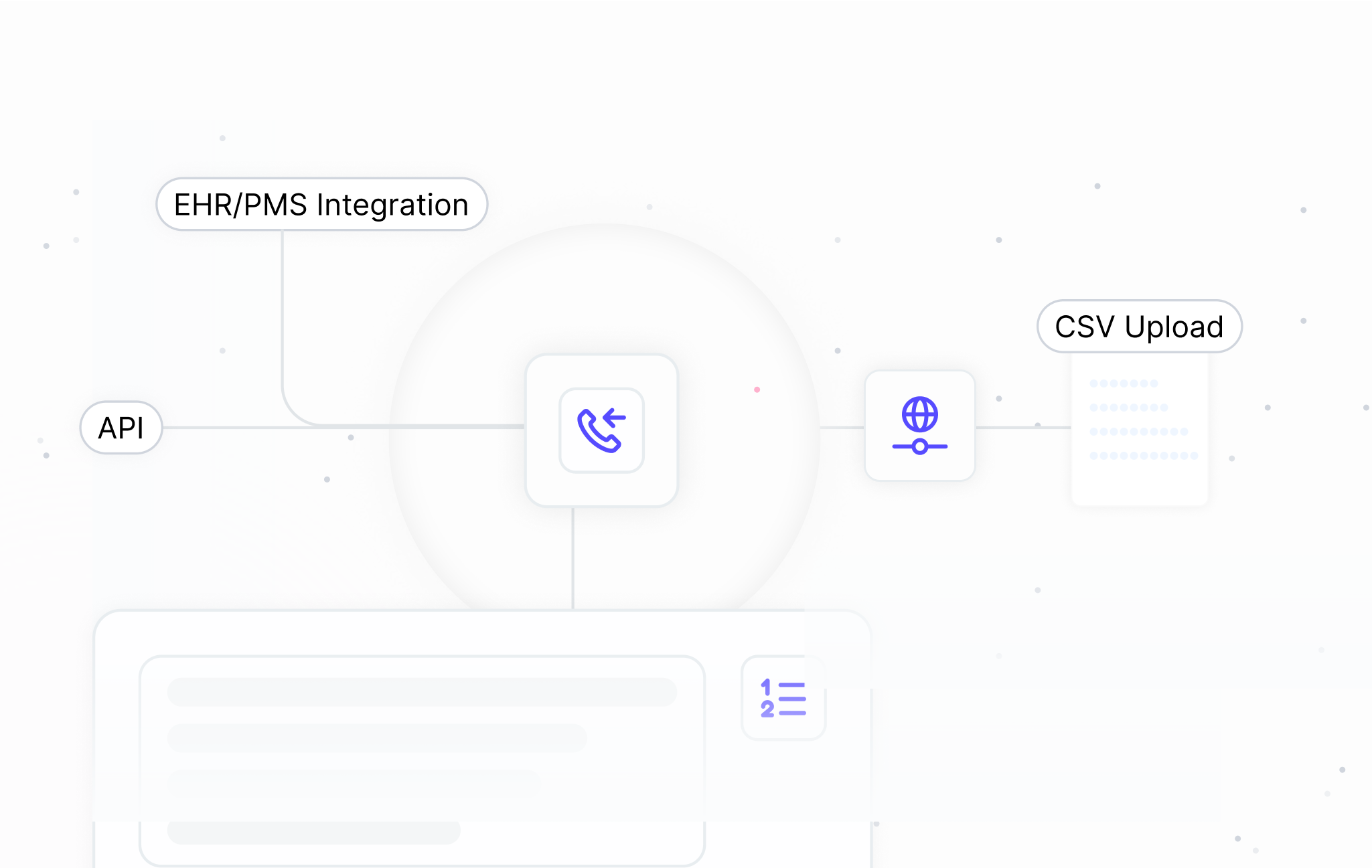
Trigger ten calls or ten thousand — either way, our flexible framework has your call script covered:
Receive the results of the calls by API or CSV, as you prefer. Results will also be available for you to view in the portal.
Place bulk calls with your data by calling our API and retrieving the results via webhook. Interested in learning more? Our team would be happy to chat.
If you’re a provider/MSO/DSO or BPO/RCM company, we’ll integrate directly with your EHR/PMS or other source of truth to automate your calls.
If you already have data handy in a CSV, simply upload your file to place calls.
Use our out-of-the-box tool to place calls with conveniently formatted columns.

SuperDial integrates with the leading EHR and PMS systems to streamline benefits verification, billing workflows, and more. These integrations minimize manual data entry and reduce administrative burden.
Book a demo


















