Medical billing is one of the most resource-intensive parts of healthcare administration. From verifying coverage to chasing claim status, staff spend countless hours on the phone with payers. For years, healthcare organizations have relied on offshore call centers to manage this workload. But with the rise of purpose-built AI voice agents, the question is no longer whether to outsource — it’s how.
This article examines the strengths and weaknesses of offshore agents compared to AI, why the industry is shifting, and what providers should consider when deciding which model to adopt.
The Challenge of Medical Billing Phone Calls
Phone calls remain a critical piece of revenue cycle management (RCM). Despite advancements in electronic transactions and portals, many claim details are only available through direct payer calls. These conversations may include verifying whether a claim has been received, confirming adjudication status, or clarifying denial reasons. For many payers, the phone is still the most reliable path to an accurate answer.
These calls are challenging for a few reasons:
- High volume: Large provider groups or dental service organizations may need tens of thousands of updates per month. Each claim requires some form of follow-up, and when scaled across thousands of patients and payers, the volume is overwhelming.
- Repetitive nature: Coverage verification, claim status checks, and prior authorizations all follow highly structured scripts. Staff often repeat the same questions hundreds of times per day.
- Time-consuming: Payer hold times can stretch into hours, creating wasted labor costs and making real-time intervention nearly impossible.
- High stakes: Each delay in obtaining accurate status directly affects AR days, cash flow, and staff productivity. Without timely updates, providers risk bottlenecks that cascade across the revenue cycle.
The combination of high volume, structured repetition, and financial impact makes billing calls both unavoidable and ripe for innovation.
Offshore Agents: The Traditional Model
For decades, offshore call centers have been the default solution for providers trying to contain costs in administrative functions. By outsourcing to lower-wage markets, healthcare organizations reduce overhead while keeping phone work in motion. This model remains widely used today, especially among organizations that lack the resources to build in-house call teams.
Advantages:
- Lower labor costs: Offshore staff are significantly less expensive than domestic employees, making it possible to manage large call volumes without ballooning payroll.
- Human flexibility: People can adapt in real time, handle unstructured responses, recognize when information is missing, and escalate unusual issues that fall outside of a script.
- Established availability: Offshore call centers are abundant, with large labor pools and established training pipelines, making it relatively straightforward to staff up quickly.
Limitations:
- Training burden: Offshore staff require extensive onboarding to learn payer-specific workflows and compliance protocols. High turnover rates mean providers often re-train from scratch, creating hidden costs.
- Variable accuracy: Miscommunications, cultural differences, and human error can compromise data integrity, leading to incorrect claim entries or missed details.
- Limited scalability: Scaling requires hiring and training more staff, which increases cost, slows ramp-up, and introduces inconsistency across teams.
- Compliance risk: Offshore operations must carefully navigate HIPAA and data security concerns, requiring heightened oversight and documentation.
While offshore agents reduce immediate staffing costs, the model often struggles with consistency, scalability, and long-term reliability. It shifts the problem from cost to quality — a tradeoff many organizations are now questioning.
AI Voice Agents: The Emerging Alternative
AI voice agents offer a fundamentally different approach: automating high-volume, repetitive payer calls using natural language processing, machine learning, and integrations with RCM systems. Rather than scaling by adding more people, organizations scale by deploying technology that can handle thousands of calls simultaneously.
Advantages:
- 24/7 availability: AI doesn’t need shifts, breaks, or overtime. Calls can be scheduled continuously, including overnight, ensuring updates are captured as soon as they’re available.
- Scalability: Once trained, AI can handle thousands of calls per month with no incremental cost per call, unlike human models that scale linearly with headcount.
- Consistency: Every AI-driven call follows the same workflow, reducing variability, minimizing human error, and producing structured data outputs.
- Auditability: Transcripts and structured data are automatically generated, simplifying quality control and ensuring every payer interaction is logged for compliance.
- Cost savings at scale: While AI requires upfront investment and integration, the marginal cost of each additional call is close to zero, making it increasingly cost-effective over time.
Limitations:
- Complex edge cases: AI may struggle with highly unstructured conversations, unusual payer workflows, or calls that require judgment beyond a script.
- Initial setup: Deploying AI requires integration with existing systems, training data, and ongoing refinement to adapt to payer nuances.
- Perception challenges: Some organizations remain hesitant to entrust revenue-critical tasks to automation, fearing disruption to established processes.
Modern AI platforms address these limitations by combining automation with human oversight. When an AI agent encounters an exception, calls can be routed to a human specialist, ensuring continuity while the AI continues to learn.
Head-to-Head Comparison
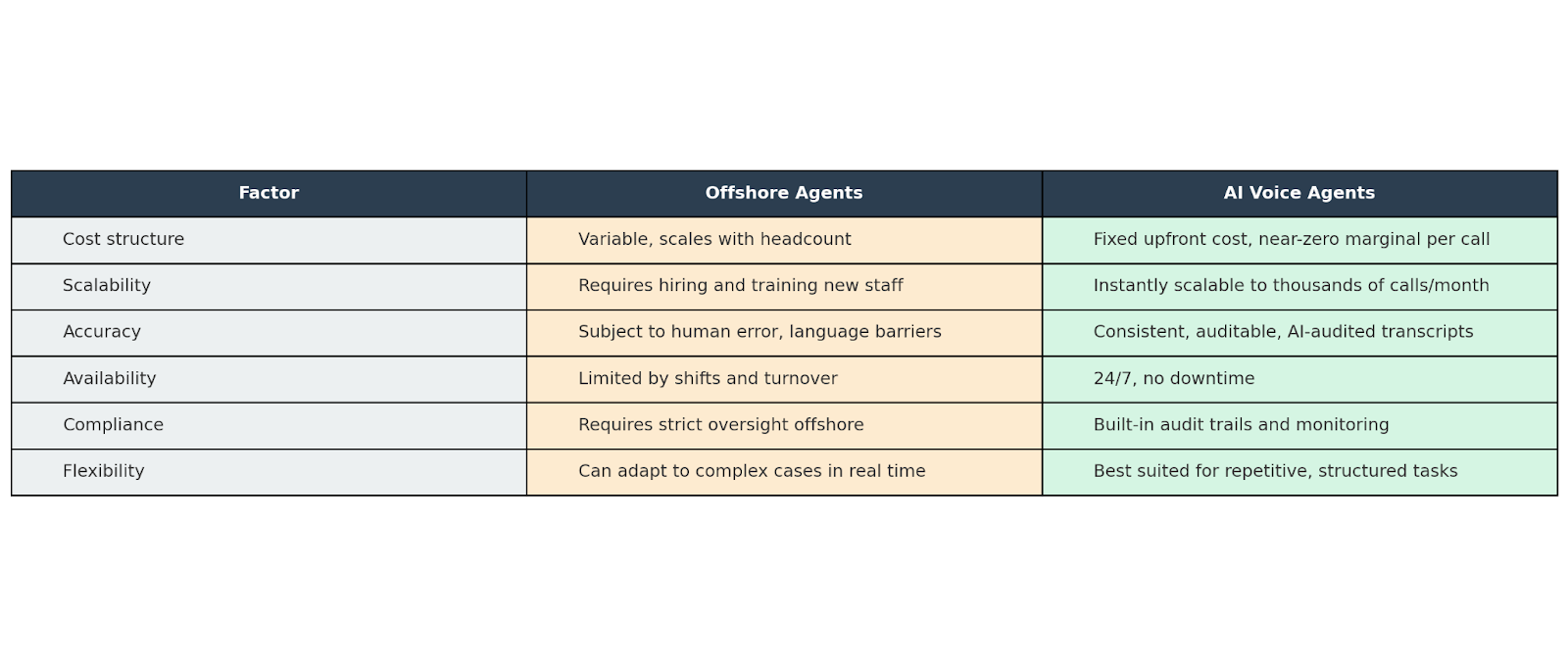
Offshore labor provides flexibility and human adaptability but at the expense of scalability and quality control. AI delivers consistency and cost savings for repetitive work but still benefits from human backup for complex calls.
Why the Industry Is Shifting Toward AI
Healthcare organizations are under intense pressure to reduce administrative costs while improving revenue cycle performance. AI fits this mandate in several ways:
- Labor shortages: Skilled RCM staff are increasingly difficult to hire and retain. Offshore models help, but AI reduces reliance on scarce labor altogether.
- Margin pressure: With reimbursement rates tightening, providers can no longer absorb bloated administrative costs. Automation offers a way to do more with less.
- Technology maturity: AI voice systems have advanced beyond static IVRs — they now navigate payer phone trees, capture structured data, and improve through machine learning.
- Demand for transparency: Automated auditing and reporting provide visibility into every call. Offshore teams rarely deliver this level of documentation without significant oversight.
This isn’t a passing trend — it’s a structural shift. As AI systems prove their reliability, the economic and operational incentives to adopt them become impossible to ignore.
The Hybrid Future: AI + Human Oversight
The reality is that AI doesn’t replace human agents entirely — it changes the distribution of work.
- AI handles the volume: Automating thousands of repetitive calls with unmatched speed and consistency.
- Humans handle the edge cases: Complex calls requiring judgment, negotiation, or payer-specific nuance are escalated to trained staff.
- Continuous improvement: Each time a human resolves an exception, that knowledge feeds back into the AI, expanding its capability.
This hybrid model provides the best of both worlds: the scalability and efficiency of AI with the adaptability and problem-solving ability of humans. Providers gain a resilient, future-proofed workflow that reduces costs without sacrificing quality.
What Providers Should Consider
When weighing AI vs offshore agents, providers should take into account:
- Volume of calls: High-volume, repetitive call workloads strongly favor automation.
- Complexity of cases: If most calls are nuanced, human support remains critical.
- Scalability needs: AI scales instantly, while offshore scaling requires hiring and training pipelines.
- Compliance requirements: AI provides detailed audit trails; offshore requires careful oversight to remain HIPAA-compliant.
- Cost trajectory: Offshore savings flatten over time; AI costs shrink as scale increases.
The decision is not binary. The most effective strategies use AI to absorb the bulk of repetitive work while reserving human expertise for where it matters most.
So What?
Medical billing phone calls remain a linchpin of revenue cycle management — but they don’t have to remain a bottleneck.
Offshore agents helped providers scale in the past, but today, AI voice agents are proving to be more scalable, more consistent, and more cost-effective for the repetitive, structured tasks that dominate payer calls. By shifting the balance toward automation while retaining humans for oversight, healthcare organizations can reduce costs, accelerate reimbursements, and strengthen compliance.
At SuperDial, we’ve built voice AI agents purpose-built for healthcare — designed to automate payer calls, audited for accuracy, and supported by human specialists when exceptions arise. The result is faster claims resolution, reduced costs, and a more resilient revenue cycle.
Ready to see how voice AI can transform your billing operations? Book a demo today.
.png)



.svg)