


Healthcare Call Center Costs by State: Why AI Is the Smarter Investment
September 24, 2025
Healthcare providers across the United States are facing mounting operational pressures. Margins are tightening as reimbursement rates shrink, staffing shortages worsen, and patient expectations climb. One of the most significant — yet often under-examined — cost centers is the call center, where teams handle scheduling, billing inquiries, insurance verifications, prior authorization follow-ups, and patient support.
These call centers don’t just represent a major line item on the P&L; they also serve as the front door to patient experience. And yet, depending on where in the country you operate, the cost of running one can vary dramatically. Because there's so much differing information on this subject, we'll try to ground this in our own experience as much as possible, offering data from case studies we've helmed, as well as insights into the more subjective aspects of state-by-state cost variance.
At SuperDial, we’ve observed this first-hand. For example, one of our clients in New York reported per-call costs nearly 2x higher than a peer organization in Texas — with no corresponding difference in patient satisfaction. This raises an urgent question for healthcare leaders: is there a smarter way to run these centers without simply doubling down on headcount?
State-by-State Cost Variability in Healthcare Call Centers
While most health systems don’t publish call center budgets, industry reports give us useful benchmarks:
- Annual cost per call center: averages $13.9M, with labor alone representing 43% (~$6M) (Hyro).
- Cost per call (CPC): averages $4.90, with some high-complexity centers reaching $10–$15 per call (T2 Group).
- Hourly agent cost: outsourcing domestically ranges between $25–$65/hour, depending heavily on geography (Nextiva).
You can see that the ranges are pretty wide. There's no doubt that state-by-state variability exists—the questions is why?
State-level variability stems largely from:
- Labor costs: higher wages and benefits in states like California, New York, and Massachusetts.
- Unionization & regulation: states with stricter labor rules or union presence drive costs higher.
- Overhead: office space in Manhattan is vastly different from office space in Oklahoma City.
- Insurance complexity: states with diverse payer mixes (Medicaid, managed care, ACA exchanges) increase call complexity and handling time.
Our Example: One California-based client reported 40% annual turnover among call center staff, leading to hundreds of thousands in retraining costs. By contrast, a peer in Florida ran with half the attrition rate and 30% lower labor overhead.
A state map visualization of average hourly call center labor costs could clearly demonstrate why geography is destiny in traditional staffing models.
The Cost Drivers in Healthcare Call Centers
Breaking down where the money goes makes the case clearer:
- Labor & Staffing
- Agents’ base pay, benefits, overtime.
- Continuous recruitment costs due to high attrition (turnover rates in healthcare call centers often exceed 30–40% annually).
- Training programs, especially for insurance complexity and HIPAA compliance.
- Agents’ base pay, benefits, overtime.
- Technology & Software
- Legacy telephony and IVR systems.
- CRM integrations.
- Workforce management tools.
- Security and audit systems.
- Legacy telephony and IVR systems.
- Overhead & Facilities
- Real estate (huge spread by state).
- Utilities, equipment, maintenance.
- Real estate (huge spread by state).
- Compliance & Regulation
- Redundant systems for HIPAA.
- Audit logs.
- Breach prevention safeguards.
- Redundant systems for HIPAA.
- Call Complexity & Handle Time
- Eligibility checks, payer escalations, prior auth follow-ups — often 20+ minutes of agent time.
- Eligibility checks, payer escalations, prior auth follow-ups — often 20+ minutes of agent time.
- Quality Assurance & Monitoring
- Supervisors and QA analysts to review calls.
- Supervisors and QA analysts to review calls.
- Peak Load Staffing
- Overstaffing required to absorb flu season spikes or open enrollment surges.
- Overstaffing required to absorb flu season spikes or open enrollment surges.
Our Example: In one RCM group we support, benefits verification calls averaged 18 minutes each when handled manually. Our AI reduced average handle time by 65%, saving the equivalent of 12 full-time agents in just that workflow.
Why AI Is the Smarter Investment
Investing in AI doesn’t just reduce costs — it creates operational resilience in ways staffing alone can’t.
- Scalability on demand: AI doesn’t require hiring surges to cover open enrollment or flu season.
- Labor cost mitigation: If labor is 40–60% of total budget, even partial AI automation creates immediate savings.
- Consistency & compliance: AI agents enforce scripts, capture structured data, and avoid common human errors.
- Experience parity across geographies: Unlike state-bound labor costs, AI delivers uniform quality nationwide.
- Data intelligence: Every AI call is logged, analyzed, and fed back into optimization loops.
Our Example: For several different companies, our AI agents now handle over 10,000 payer calls every month, including benefits verification, claims status, and prior auth follow-up. Each call would have otherwise required a human to wait on hold, navigate payer portals, and log results.
How AI Transforms Key Call Center Functions
Anyone still assigning humans with the rote tasks of appointment scheduling, eligibility checks, prior auth follow up, patient reminders, etc. is wasting their time and money.
AI has already moved on!
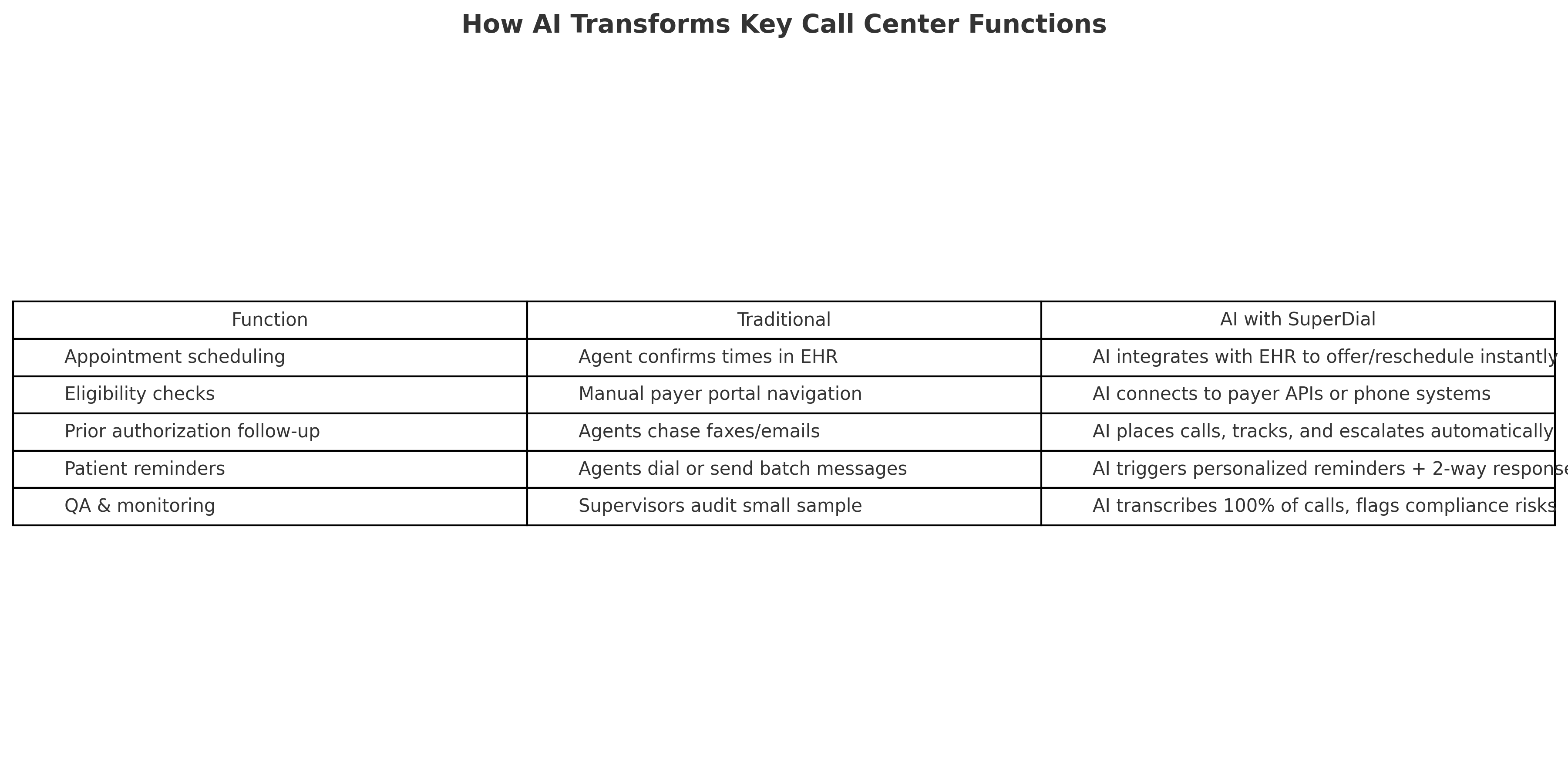
Our Example: At a large dental support organization, our AI agents now complete 70% of eligibility verification calls end-to-end without escalation, cutting costs and dramatically improving turnaround time.
Quantifying the ROI & Cost Savings
There are lot of ways to talk about potential cost savings, especially when they vary state to state, but the numbers don't lie. The ROI argument is strongest when framed numerically:
- 30% cost reduction in healthcare call centers is achievable through AI (Simbo.ai).
- Per-interaction costs can fall from $5.60 to $0.40.
- Labor savings of $145k–$215k/month reported in healthcare AI call pilots (Impact Advisors).
- $500M+ in savings in enterprise call centers demonstrated by Microsoft’s AI adoption (Reuters).
Our ROI Example: One of our clients handling 10,000 calls/month had a baseline cost of ~$5 per call. After implementing SuperDial's AI agents, the effective cost per call dropped below $2. Annualized, that represents a savings of $360,000.
Structural & Practical Considerations
This is not the only paradigm shifting in the industry now. While the ROI is clear, healthcare leaders should plan for:
- Change management: staff may resist automation unless positioned as augmentation, not replacement.
- HIPAA & compliance: AI must meet SOC 2 and HIPAA safeguards (SuperDial is both).
- Integration lift: AI must tie into EHR, CRM, payer APIs, and legacy PBX systems.
- Fallback to humans: AI escalation protocols ensure nothing falls through the cracks.
- Continuous tuning: payer rules and insurance workflows evolve constantly — models must stay up to date.
Our View: We’ve seen projects fail when leadership underestimated staff retraining. The most successful rollouts included workshops where staff learned how to collaborate with AI — freeing them to handle the complex, empathetic calls.
Forecast & Trends
If you zoom out to a wider view of the impact of AI on healthcare revenue cycle management, we're only at the beginning of an upward exponential curve. Let's take a look at some of the longer term changes ahead:
- Agentic AI (autonomous agents that execute multi-step tasks) will move beyond scripts into real claim resolution.
- AI-to-AI conversations between payers and providers will reduce call volume entirely.
- Hybrid models (AI for tier-1, humans for escalation) will become the industry standard.
- Regulators will soon mandate AI audit trails and explainability.
- Cost declines in compute will make AI accessible even for mid-sized practices and regional hospitals.
Our View: We expect AI-to-AI calls — our bots calling payer bots — to become mainstream within the next 2–3 years. This will transform revenue cycle management and render “hold times” obsolete.
Why It Matters
Healthcare call center costs vary dramatically by state, but they all share one problem: they are too high, too labor-intensive, and too inconsistent to be sustainable in the long run. AI offers not just a cost reduction, but a strategic path to more consistent, compliant, and patient-friendly operations.
SuperDial has already shown how AI can reduce per-call costs by more than half, eliminate thousands of wasted staff hours, and provide call quality monitoring at scale.
If you want to see how much AI could save your call center, request a SuperDial demo today. We’ll build you a custom state-by-state cost comparison and show exactly how much you could save by replacing wait times with AI.


