When it comes to revenue cycle management (RCM), speed and visibility are everything. The longer a claim’s status remains unclear, the longer valuable revenue sits in limbo. A single delay in communication can cause cascading effects: extended accounts receivable (AR) days, strained staff resources, and difficulty forecasting financial performance.
Unfortunately, many healthcare providers still face slow, inconsistent, or incomplete claim status updates from insurers. Outdated systems, fragmented communication, and payer variability create significant challenges. But with the right processes and technology in place, you can dramatically accelerate how quickly you get claim status information — and more importantly, how much you can trust it.
This guide outlines practical steps to streamline the process, eliminate friction, and build a faster, more predictable revenue cycle.
Why Claim Status Updates Matter More Than Ever
Claim status updates may feel like a small administrative detail, but they sit at the heart of financial stability. Without timely updates, providers are left in the dark:
- Revenue is delayed: Without visibility, claims languish in AR, tying up cash that could be reinvested into staffing, equipment, or patient care.
- Staff are overburdened: Teams spend hours chasing down information by phone or portal, reducing their capacity for high-value work.
- Denials pile up: Delayed updates make it harder to spot problems early. By the time a denial is confirmed, it’s often too late to intervene effectively.
- Patients lose trust: When providers don’t have clear answers on claim status, patients feel the uncertainty firsthand.
Faster claim status updates don’t just improve efficiency — they enable better financial performance, better resource allocation, and better patient experiences.
1. Diagnose the Roadblocks
Before you can improve, you need to understand what’s slowing you down. Some of the most common barriers include:
- Electronic data gaps: Even with EDI transactions (276/277), updates are often incomplete or inconsistent, leaving staff with partial answers.
- Payer variability: Each insurer has its own approach to transmitting claim information, from formatting quirks to entirely different systems.
- Manual follow-ups: Many organizations still rely on staff to call payers directly — a process plagued by long hold times, repetitive data entry, and inevitable human error.
- Fragmented systems: When data comes in from multiple portals, phone calls, and EDI feeds, it’s hard to consolidate into a single source of truth.
Mapping these friction points will help you target improvements where they matter most.
2. Maximize Electronic Data First
The industry-standard way to obtain claim updates is through electronic eligibility and status checks. But simply having access to 276/277 transactions doesn’t guarantee efficiency. To get the most out of these feeds:
- Automate retrieval: Instead of pulling claim status on an ad hoc basis, set up automated schedules that align with payer response times.
- Integrate results: Feed data directly into your RCM platform to eliminate manual rekeying and reduce the risk of transcription errors.
- Flag gaps early: Build rules to highlight missing or contradictory fields so staff can intervene before those gaps become bottlenecks.
- Prioritize exceptions: Instead of manually reviewing every claim, train your system to escalate only those with incomplete, delayed, or concerning status codes.
Electronic data alone won’t solve the problem, but properly structured, it reduces unnecessary manual effort and creates a baseline of visibility.
3. Automate Phone Calls at Scale
Despite advances in EDI, phone calls remain the most reliable way to confirm claim status. The challenge is scalability. Calling payers is tedious, slow, and expensive when left entirely to staff. This is where automation makes a measurable difference:
- Voice AI agents can navigate payer phone trees, wait on hold, and capture structured data at scale.
- Fallback systems ensure that when automation encounters an exception, calls are routed to human staff rather than abandoned.
- Quality layers audit call transcripts for accuracy so that the data you receive is actionable.
By offloading routine phone calls to automation, staff are freed to focus on higher-value work such as denial prevention, complex appeals, and patient financial counseling.
4. Centralize and Standardize Claim Data
Fast claim updates only create value if your team can trust and act on them. For many organizations, the challenge is less about speed and more about usability. Best practices include:
- Consolidate into one dashboard: Bring EDI feeds, phone call results, and portal data into a single view that staff can rely on.
- Standardize formats: Normalize payer-specific quirks so claims are displayed consistently regardless of source.
- Enable drill-down: High-level dashboards should link directly to detailed claim notes, transcripts, or status codes for context.
- Surface insights, not just data: Instead of dumping raw status codes, translate them into actionable next steps (e.g., “Claim requires documentation” rather than “Status 21”).
A unified, actionable data layer prevents confusion and ensures your team can resolve issues faster.
5. Monitor the Right Metrics
Improvement requires measurement. Tracking the right KPIs helps you gauge progress and identify where further optimization is needed. Consider monitoring:
- Average AR days before and after new processes
- Volume of claims requiring manual follow-up versus automated completion
- Staff hours saved each month on claim status checks
- Denial rate reduction due to earlier interventions
- First-pass resolution rate as an indicator of overall claim cycle health
Measuring these outcomes allows leadership to prove ROI, secure buy-in for further investment, and continuously refine processes.
6. Build for Resilience, Not Just Speed
It’s tempting to focus only on faster turnaround times, but true improvement means building resilience into your RCM process. That means:
- Redundancy: Having multiple pathways for claim updates (EDI, phone, portal) ensures continuity if one channel fails.
- Continuous learning: Feeding new payer rules, exceptions, and outcomes back into your system improves accuracy over time.
- Scalability: Processes that work for 1,000 claims a month must scale to 10,000 without additional headcount.
- Compliance focus: Every solution must preserve HIPAA compliance and meet data security requirements while improving efficiency.
Resilient processes ensure that faster claim updates aren’t just a short-term win but a sustainable advantage.
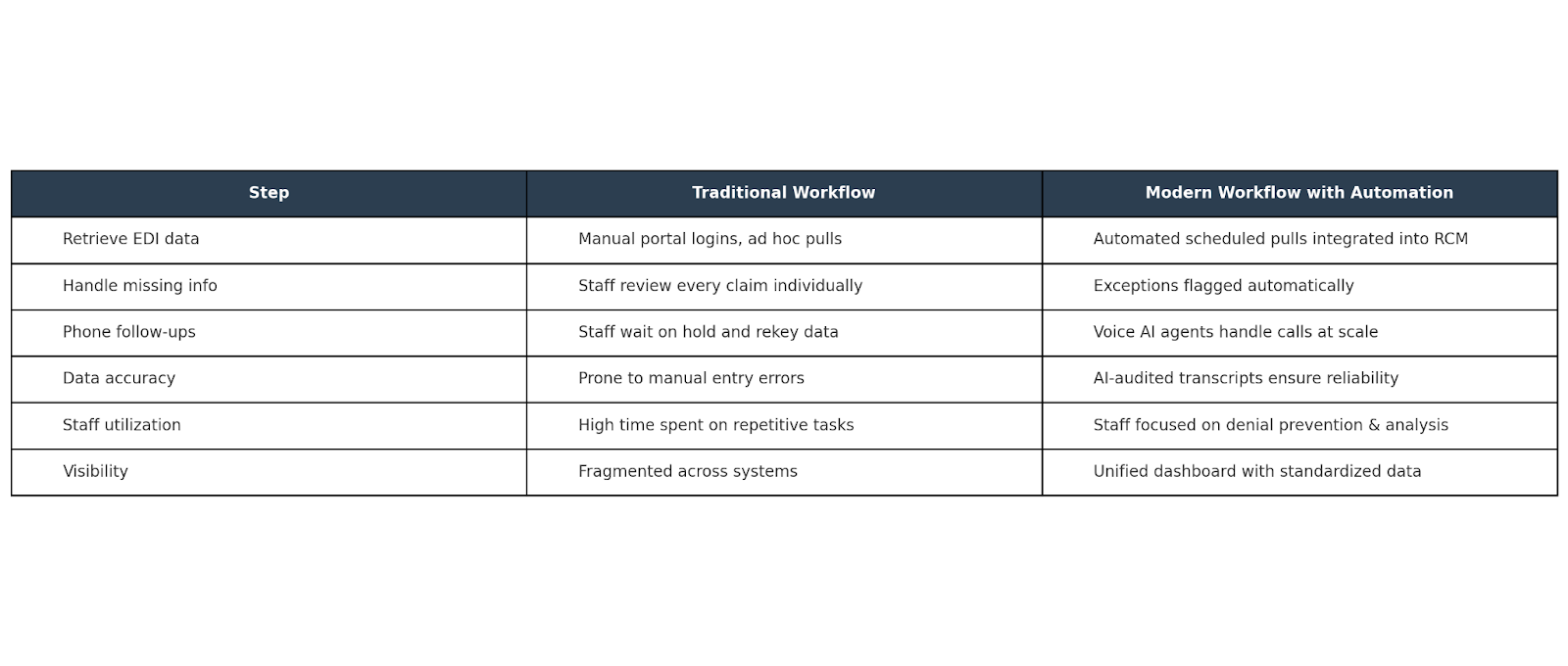
Practical Comparison: Traditional vs. Modern Claim Status Workflows
So What?
Faster claim status updates aren’t just a “nice to have” — they’re a prerequisite for financial stability in healthcare. When providers can see, trust, and act on claim information quickly, they reduce AR days, protect margins, and improve patient experiences.
The path forward is clear:
- Eliminate gaps in electronic data.
- Automate payer phone calls at scale.
- Standardize and centralize claim updates.
- Track performance and continuously improve.
At SuperDial, we believe automation should empower staff, not replace them. By combining voice AI agents with intelligent auditing and human oversight, we help providers achieve faster claim updates without adding headcount — turning what was once a bottleneck into a competitive advantage.
Ready to accelerate your revenue cycle? Book a demo and see how faster, more reliable claim updates can transform your operations.
.png)



.svg)