In medical billing, every phone call matters. Whether it’s verifying coverage, checking claim status, or resolving denials, calls with payers are essential to keeping the revenue cycle moving. But too often, these calls end without answers — forcing staff to call back, escalate, or rework claims.
This is where call resolution rate comes in. It measures the percentage of calls that are fully resolved on the first attempt, without the need for follow-ups. A higher resolution rate means faster reimbursements, lower administrative costs, and less strain on staff.
In this guide, we’ll break down why call resolution matters, common barriers to achieving it, and practical strategies to improve resolution rates across your billing workflows.
Why Call Resolution Matters in Medical Billing
The call resolution rate is more than a customer service metric — in revenue cycle management (RCM), it directly impacts financial performance.
- Shorter AR days: When calls are resolved quickly, claims move through the system faster, improving cash flow.
- Reduced labor costs: Each unresolved call adds to staff workload. Higher resolution means fewer repeat calls, freeing time for other tasks.
- Improved accuracy: Calls that end with complete, trustworthy information reduce rework and prevent denials downstream.
- Staff productivity: High-resolution processes reduce burnout and turnover by minimizing repetitive, frustrating follow-ups.
In short: better resolution translates directly into financial and operational stability.
Common Barriers to High Call Resolution
Despite best efforts, many organizations struggle with low resolution rates. The most common causes include:
- Incomplete or inconsistent data
Payers often provide partial answers electronically or over the phone, leaving staff without enough information to move forward. - Complex payer workflows
Each insurer has its own IVR, terminology, and requirements, making it hard for staff to navigate consistently. - Manual processes
Staff manually take notes, rekey data, and escalate unclear responses, creating room for error and slowing resolution. - Training gaps and turnover
Offshore or newly hired staff may not have the depth of knowledge needed to resolve calls efficiently. High turnover exacerbates the problem. - Limited quality control
Without auditing or monitoring, unresolved calls slip through unnoticed until AR days pile up.
Understanding these barriers is the first step toward fixing them.
Strategies to Improve Call Resolution Rates
1. Standardize Call Scripts and Workflows
One of the most effective ways to improve resolution is to standardize the process. That means:
- Developing payer-specific scripts that guide staff through all required questions.
- Training staff to recognize payer-specific codes, terminology, and nuances.
- Creating checklists to ensure no critical data points are missed.
Standardization reduces variability across agents and ensures every call captures the full picture.
2. Leverage Automation for Repetitive Calls
Many payer calls follow highly structured workflows. Automating these calls with AI voice agents increases consistency and efficiency.
- AI can navigate IVRs, ask scripted questions, and capture structured responses without fatigue or error.
- Automated systems ensure complete data capture, improving the likelihood of resolution on the first attempt.
- Human staff can step in only when exceptions occur, reducing the burden of repetitive work.
This hybrid approach boosts both resolution rates and scalability.
3. Improve Data Integration and Accessibility
Even when calls are successful, resolution falters if staff don’t have immediate access to the data. To close the loop:
- Integrate call transcripts and structured outputs directly into your RCM or practice management system.
- Provide dashboards that consolidate payer responses for real-time visibility.
- Use alerts to flag incomplete or contradictory information before it affects claim submission.
The goal is simple: the right data, in the right place, at the right time.
4. Establish a Robust Quality Assurance Process
Quality assurance ensures that unresolved calls don’t slip through unnoticed. Best practices include:
- Auditing a sample of call transcripts weekly for completeness and accuracy.
- Using AI-powered auditing tools to flag gaps automatically.
- Providing regular feedback and refresher training to staff based on audit findings.
Continuous monitoring creates a feedback loop that steadily improves resolution performance.
5. Track and Act on Resolution Metrics
You can’t improve what you don’t measure. Establish KPIs to monitor and refine your call resolution strategy:
- Resolution rate: Percentage of calls resolved on first attempt.
- Repeat call rate: Percentage of calls requiring follow-up.
- Average handling time: How long calls take to resolve.
- Denial prevention impact: Reduction in denials attributable to better call resolution.
Regular reporting on these KPIs makes it easier to identify bottlenecks and measure ROI.
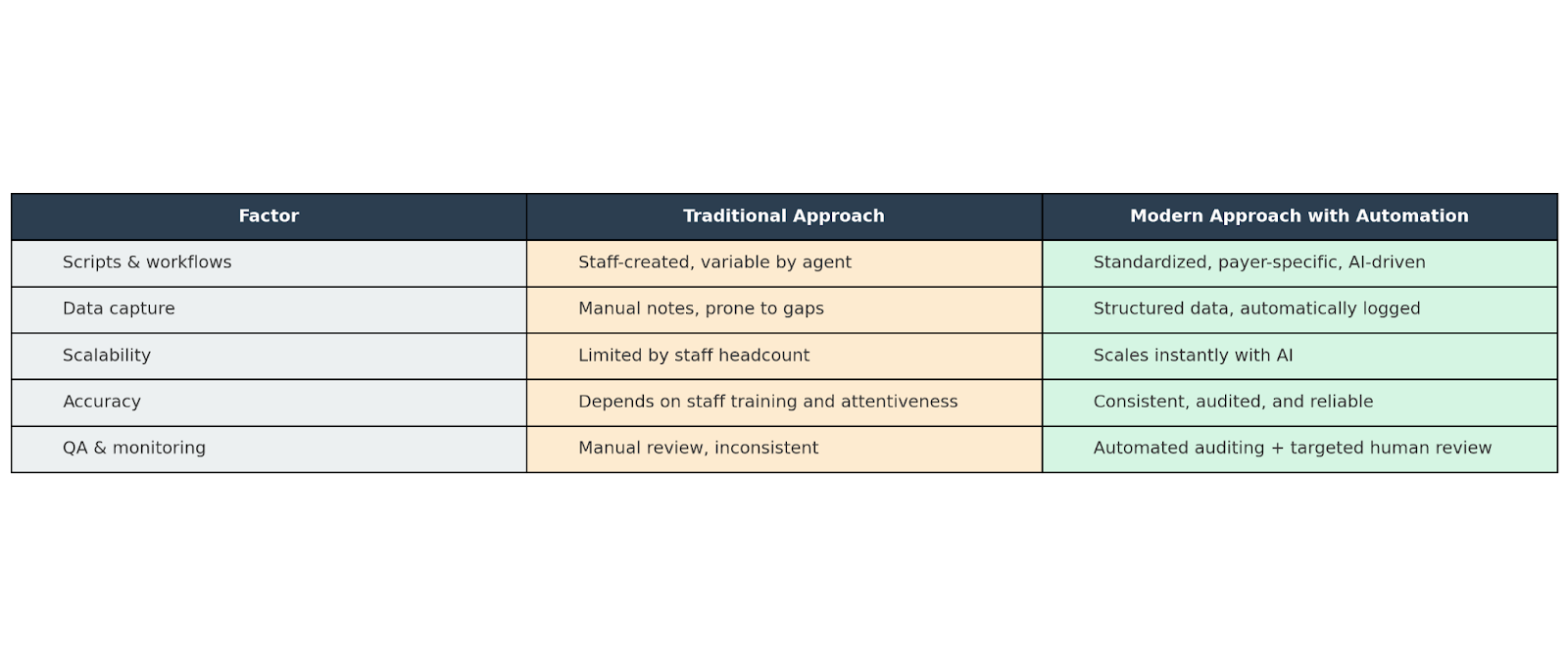
Traditional vs. Modern Call Resolution Approaches
The Bigger Picture: Building Resilient Workflows
Improving call resolution rates isn’t just about reducing callbacks — it’s about creating a more resilient RCM process. High-resolution workflows mean:
- Faster reimbursements and fewer denials.
- Better use of staff time and less burnout.
- Stronger compliance through auditable, standardized processes.
- A more predictable revenue cycle, even under labor shortages or high claim volumes.
By focusing on resolution, providers move from reactive to proactive — catching issues early and resolving them before they snowball into bigger problems.
Conclusion
Low call resolution rates are a silent drain on revenue cycles. Every unresolved call adds to AR days, staff frustration, and operational inefficiency.
The solution is a combination of standardization, automation, integration, and quality assurance. By embracing modern approaches — especially AI-powered call automation — providers can dramatically improve resolution rates, reduce costs, and build a more resilient revenue cycle.
At SuperDial, we’ve built voice AI agents designed specifically for healthcare billing workflows. Our technology automates repetitive calls, audits every interaction, and integrates seamlessly with your systems — helping providers achieve higher resolution rates at scale.
Ready to improve your call resolution rate? Book a demo today.
.png)



.svg)